Another article in the trauma-informed series by Dr. Teresa Camille Kolu, Ph.D., BCBA-D
In relationships we do rituals.
“BLECH!” Startled, I looked down at my sweet, expressive daughter with a true disgust face. Everybody laughed. I was kinda mortified but I laughed too. The woman at MeOhMyCoffeeAndPie (you HAVE to go) had just answered her question with “it’s sauteed onion” when my kid asked “what’s the scone flavor today?”
Ok, I guess she wasn’t expecting that.
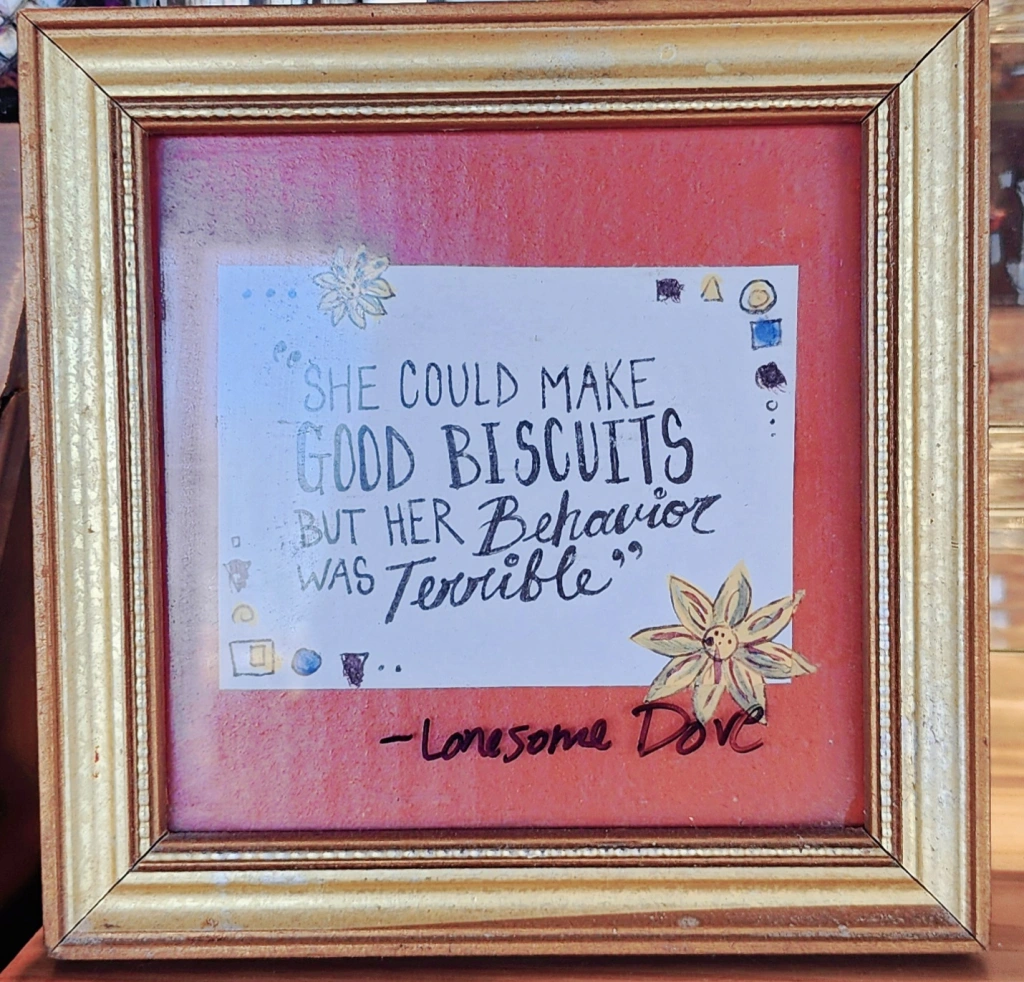
I was too caught up noticing this awesome tiny, framed quote by the display case. As a young reader I LOVED Larry McMurtry, see, who wrote Lonesome Dove and a whole lot more. He and I both went to UNT (decades apart, of course) where he gave us a wonderful author meet and greet (early 90s for me, when this kid was not even a twinkle). The coffee and pie shop had quite appropriately chosen to frame this gem of a quote: “She made great biscuits, but her behavior was TERRIBLE”.
My daughter and I were out doing a ritual Saturday thing. My mom used to sing “Come Saturday Morning” with me (we had the sheet music, so it was right up there with “Country Roads” and “The City of New Orleans” in my book). And sometimes we would spend time just us, and I would look at her hands and sing this song in my head. Saturday mornings, for a couple precious hours, are time when my daughter doesn’t have to share me with her little brother, and she pays me back by asking me questions I can’t answer. It’s at this time I learn that even 5 year olds wonder things about God and the universe, have nightmares, they can have crushes, they have fears, they might still want to hold my hand.
I LOVE biscuits but I love her even more. I love her more than her behavior, even that sort of behavior that makes you want to fire the babysitter just so you’ll never have to greet that face that saw the terrible behavior you thought your kid would never do in public and after all, you are a behavior analyst! (Do I think it’s easier because I’m a behavior analyst, my new friend asked recently? Heck no. I personally think it’s harder. But I do think being a parent has made me a better behavior analyst.)
So in relationships we do rituals, like setting up meaningful goodbyes when we leave the room, or when rhythms change and we won’t be spending as much time together anymore. If not, we leave devastation.
When I watch animals grieving each other’s deaths… especially horses and dogs… I notice how fully present they are for the goodbye.
And I am always grieved to consider the implication: such a meaningless slog of goodbyes without reason, or participation, we inflect this on clients when caseloads shift; when a therapist moves; when a client with certain behaviors moves into Hall B, so we just HAVE to abruptly move Client A into Hall D, so they won’t antagonize each other and never mind Client A will never again see her best friend client, or even the janitor—who was like a mother to her and had been there for 12 of the client’s 15 years in this mental facility again.
We often have to make hard decisions, but we should ask questions (“what really hurt your feelings this past week? Today?”) because in relationships we apologize when we’re wrong.
When we realize we hurt others, we shift so that we won’t keep doing the hurtful thing.
My mom remembered the pain of being hurried as a child. I knew that, and I forgot it. I remembered it again this month when I was going through an exercise I was making for a new workshop we will offer at cuspemergenceuniversity.com. The exercise has us grownups go through questions that reveal the triggers for us – the things in our everyday situations that make us more likely to react swiftly (often in a hurtful way) to the others around us. And I realized two things: being hurried doesn’t feel good to children, and hurrying children doesn’t feel good to adults. So what do we do? This week, maybe you will notice a ritual that is always done with urgency, and think, how does this feel? What would this feel like if I slowed down? Now, the harder part: What would it take for me to build in space around this… ten extra minutes before it, so that we don’t have to experience this, every single time, in hurried mode? I tried this, and my children really love it, although I won’t hear about it from them. Their lingering hugs (mama, don’t let go first!) and their wonder as we have time to look around the yard for a new flower before we buckle our seatbelts… the absence of urgent reminders and exasperated sighs… perhaps even a reduction in tense moments when I’m about to lose it and yell. These changes are rewarding enough for me to keep doing this. Because I love them more than biscuits.
Yes, rapport is often transactional. Although it was by design at first, it doesn’t always have to be that way. I talk about this just a little bit in my buffers article, in the relationship section. And in the trauma sensitivity course we talk a little about how to be more sensitive to what folks go through (including your staff) so that YOU can be a little less harsh, a little more supportive, around things you didn’t even realize were hurting the other person.
In relationships, we apologize; we give freely; we do things uncontingently (yes, I know you won’t be able to look that up, and there’s a reason- we talk about it more on instagram and it bears more attention); and we are generous with things the person really needs, like time, kind words, and those little rituals that they consider special. Have you ever worked with a therapist the client really adored? Or a professor beloved by their students? I remember two. The professor is loved and really loves. She gives generously of her wisdom, time, and appreciation for students. (You wanted to ace her class and reflect what you admired in her, even as she whispered the things that made you more of yourself, more creative and passionate and able to grow confidently in the direction of your dreams.) The other person I remember is a therapist who had kids riding on her shoulder at recess in our mixed school for kids with developmental differences and peers. And those folks taught me that you can have instructional control when it’s time, and still have fun with the people who look up to you. Rapport IS often transactional. But the relationship doesn’t have to be.
Thanks for reading.
Oh… and I personally think, in the Longmont area, that Lucille’s has the best biscuits.
And OhMeOhMyCoffeeAndPie has the best lemon bars, if you’re wondering.
I love you more than biscuits, daughter of mine. And I love you even when your behavior is terrible.




